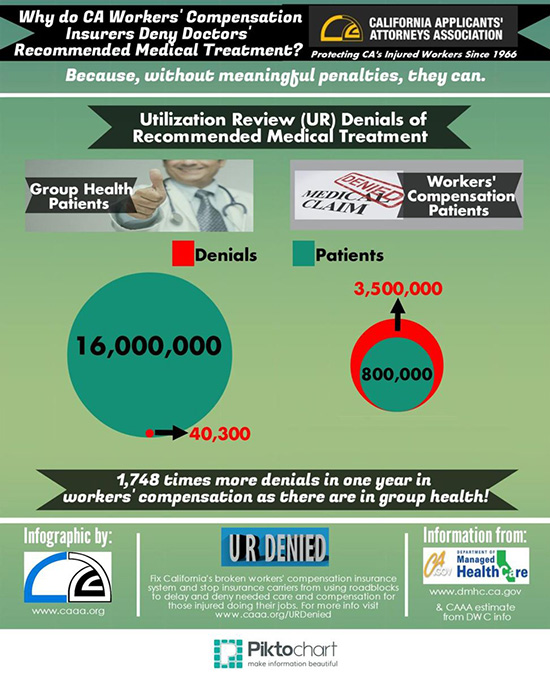
Today, CAAA releases the second infographic in our series comparing medical care, UR, IMR, amount spent on overhead and other measures of quality patient care in group health vs. workers' compensation insurance.
California's workers' compensation insurance system suffers in comparison.
There are problems with group health insurance, but they are nothing compared to California workers' compensation insurance.
Today, we continue the comparison by showing the avalanche of Utilization Review (UR) denials in workers' compensation - more than 1,748 times that of group health, for 15 million fewer patients!
We know that this unjustified constant denial by UR is a concerted effort by insurers to delay and deny paying for doctors' recommended medical care.
Please share this important infographic with your digital networks TODAY!
Here are three ways you can share the infographic digitally:
- Share on Facebook:
- Click the following link to direct you to: CAAA's Facebook Page
- View the infographic post on the right hand side of the page.
- Underneath the infographic click "like" and then click "share" to share the post to your Facebook network.
- Share on Twitter:
- Click the following link to direct you to CAAA's Twitter Page
- View the infographic tweet under the heading "Tweets" in the center of the page.
- Underneath the infographic click the conjoining arrow symbol
 to retweet the tweet to your Twitter network.
to retweet the tweet to your Twitter network.
- Share by forwarding this e-mail with the infographic shown below:




No Comments
Leave a comment